What Are Plantar Warts?
Plantar warts, which predominantly surface on the feet, owe their origin to the human papillomavirus, commonly called HPV. Out of the extensive spectrum of over 100 identified HPV strains, only a select few are culpable for inducing plantar warts. To fully appreciate the root causes, it's crucial to discern the environments in which this virus thrives and the typical avenues of transmission.
HPV relishes warm, humid conditions. This predisposition explains why communal areas with such climates, like public showers and swimming pools, are often hotspots for transmission. The damp floors of these amenities provide an ideal breeding ground for the virus. Individuals walking barefoot in these locales unwittingly expose their feet to this lurking threat, especially if there are minute cuts or abrasions. Therefore, navigating these moist areas without protective footwear significantly elevates the risk of contracting the virus.

Direct contact stands out as a potent vector of transmission. When an individual comes in contact with a wart on another person or uses items that have been in contact with warts, such as towels or shoes, the virus can be transferred. It's not merely the visible warts that pose a threat; sometimes, virus particles from affected individuals can be present on surfaces they've touched, making transmission possible even without a visible wart.
The strength and responsiveness of one's immune system play a pivotal role in determining susceptibility. While the virus might be ubiquitous, not everyone who comes into contact with it develops warts. People with weakened, compromised immune systems, whether due to medical conditions, medication, or age, are more vulnerable to contracting warts. Their bodies might not mount an effective defense against the virus, thus leading to the manifestation of plantar warts.
Causes of Plantar Warts
Recognizing and understanding the symptoms associated with plantar warts is essential for early detection and effective treatment. These growths are distinguishable from other foot-related anomalies thanks to specific indicators, ensuring the use of the proper interventions.
First and foremost, plantar warts often present as hard, grainy growths. Predominantly located on the soles of the feet, these growths are particularly noticeable on the heels or balls. Unlike other skin outgrowths, they bear a rough texture and may resemble a callus. Their location often subjects them to pressure from standing and walking, which can further compact the growth, making them firmer.
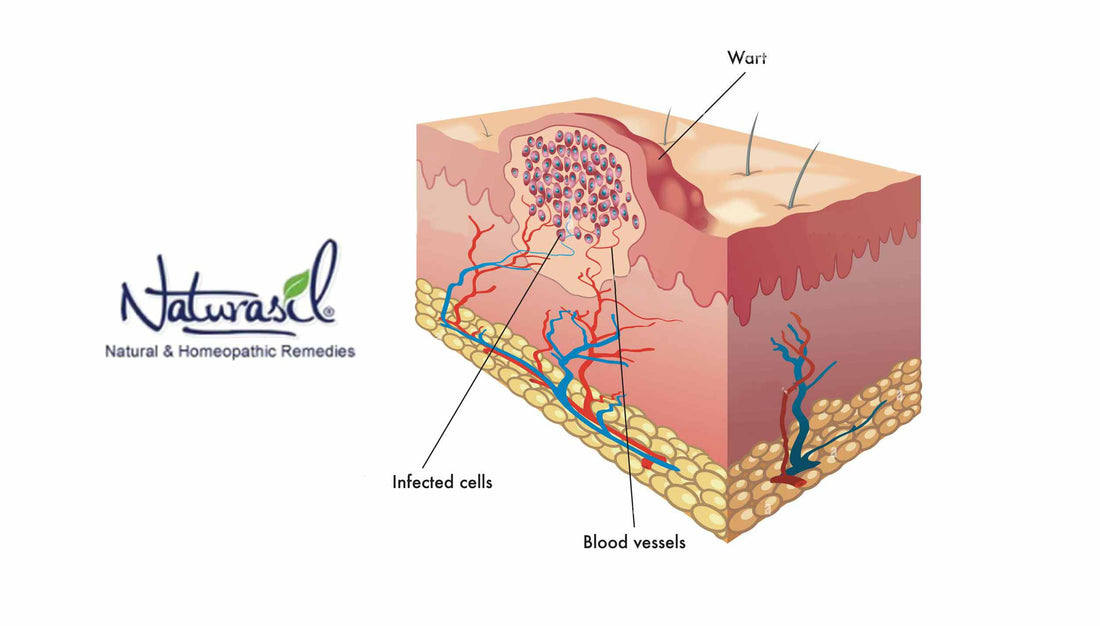
The second distinguishing trait of plantar warts is the presence of tiny black dots within the growth, colloquially termed 'wart seeds.' Contrary to the name, these are not seeds or any form of propagation. In actuality, these pinpoint black spots are clotted blood vessels. They form due to the pressure exerted on the warts, leading to minor bleeding into these growths. These spots, visible upon close examination, provide a valuable diagnostic clue.
Finally, individuals with plantar warts commonly report a persistent sensation of pain or tenderness when walking or standing. This discomfort arises as the wart's growth subjects the underlying structures of the foot, particularly nerves, to pressure.
Given these symptoms, it's imperative to highlight that plantar warts can be easily confused with other foot conditions, especially corns or calluses. Both can manifest as toughened skin areas on the feet. However, the absence of the hallmark black dots and the specific pain pattern make a marked distinction. If any ambiguity arises in distinguishing these conditions, it is paramount to consult a medical professional. A dermatologist, in particular, can provide clarity and guidance on the appropriate course of action.
Recognizing the Symptoms
The accurate identification of plantar warts is paramount for their effective management. While many cases can be ascertained through a simple visual assessment, certain ambiguous situations necessitate a deeper and more comprehensive diagnostic approach. In these instances, specific clinical techniques can demystify the presence of warts and guide subsequent treatment measures.
A physical examination spearheads the diagnostic process. A dermatologist conducts this examination, which entails a thorough examination of the suspected area. The wart's size, shape, and texture provide initial cues. A key feature of plantar warts is the presence of characteristic black dots indicative of clotted blood vessels. To better visualize these, a dermatologist might delicately trim the uppermost layer of the wart. This action confirms the diagnosis through the revelation of these telltale signs and offers relief from any associated discomfort.
A Dermatoscope is the tool of choice if the diagnosis remains equivocal after the physical examination. Dermoscopy, the procedure involving this instrument, magnifies the skin's surface, providing a detailed view of its architecture. The enhanced visibility aids in discerning subtle features that might be indiscernible to the naked eye. In the case of plantar warts, dermoscopy can reveal the intricate vascular pattern and the distribution of the aforementioned black dots, further cementing the diagnosis.
However, a biopsy may be deemed necessary in extremely rare scenarios where the diagnosis remains clouded or when there's suspicion of another underlying condition. This invasive procedure involves excising a small fragment of the suspicious growth. This tissue sample is sent to a pathology laboratory for rigorous microscopic analysis. Histological examination can definitively differentiate a wart from other skin conditions and malignancies, ensuring that the patient receives the most appropriate care.
Preventing Plantar Warts
Plantar warts, while often benign, can bring about significant discomfort and cosmetic concern. Prevention, paramount in health care, offers the most effective strategy against these stubborn growths. By understanding and adopting specific preventive measures, one can significantly reduce the risk of contracting the causative human papillomavirus (HPV) and subsequently developing plantar warts.
Firstly, avoiding direct contact with an existing wart is imperative, be it on oneself or others. The HPV strains responsible for plantar warts are highly contagious. Touching a wart or even being in contact with surfaces or objects that have come into contact with it can easily facilitate the transfer of the virus. Such direct transmission is a common pathway for the spread of this condition.
Furthermore, public places, especially warm and damp ones, are notorious breeding grounds for HPV. Places like communal showers, gym locker rooms, and public swimming pools see a high footfall, increasing the probability of the virus lingering on the floors. To mitigate the risk in such environments, always wear footwear. Sandals, flip-flops, or water-resistant shoes can act as a protective barrier, preventing direct exposure of the feet to virus-laden surfaces.
Moist environments exist in public places and can develop within one's shoes, especially after prolonged wear or physical activity. HPV thrives in moisture, making it essential to keep the feet dry. If socks become wet from sweat or external water, change them immediately. Regularly drying the feet and opting for moisture-wicking socks can reduce the risk.
Lastly, for those who already have a wart, it's crucial to avoid picking or scratching it. Manipulating a wart can release viral particles, infecting other areas of the same foot, the opposite foot, or even other individuals. A hands-off approach ensures the containment of the virus at the already-affected site.
Treatment Options
Plantar warts, while typically non-malignant, can pose both discomfort and aesthetic concerns. Once accurately identified, exploring the range of available treatment options becomes essential. These interventions, ranging from topical applications to more invasive procedures, aim to eradicate the wart and alleviate associated symptoms.
Over-the-counter salicylic acid products are widely available and have proven efficacy. This compound facilitates the shedding of the wart by dissolving the keratin structure that constitutes it. With consistent application, salicylic acid can gradually diminish the size of the wart, eventually leading to its complete resolution. However, following the application instructions is essential to preventing skin irritation.
For warts resistant to topical treatments, cryotherapy emerges as a viable option. A healthcare professional administers this procedure, which involves applying liquid nitrogen to the wart and freezing its cellular structure. The extreme cold induces cell death in the wart, which then sloughs off over time. While highly effective, cryotherapy might require multiple sessions and can be associated with transient discomfort.
When warts prove particularly tenacious, minor surgery is a potential course of action. This procedure, typically conducted under local anesthesia, involves the wart's excision, ensuring the entire growth's removal. The benefit of surgical removal is immediacy, eliminating the warts in a single session. However, post-procedural care is crucial to prevent infections and ensure optimal healing.
Lastly, laser treatment offers a modern approach for those seeking advanced interventions. The laser targets the wart, utilizing a concentrated light beam that eventually destroys it. While highly precise, laser treatments may necessitate multiple sessions and can come with a higher price tag.
Conclusion
Plantar warts, predominantly benign, often serve as a source of notable discomfort and concern. Understanding their origins, manifestations, and diagnostic techniques is instrumental in providing timely interventions and staving off their recurrence. Many options exist for Plantar Wart treatment. For those seeking how to remove Plantar Warts, the solution often lies a click away, emphasizing the value of expert solutions in this domain. Nevertheless, liaising with a seasoned dermatologist or healthcare professional when in doubt about any skin anomaly remains pivotal, ensuring one receives the gold standard in care and advice.